Thanks to a complete team effort — from a quick-thinking security guard to the precise talents of an expert interventional cardiologist — Bill Gruber got a second chance at life.
Bill Gruber was determined to avoid his family history of heart disease. His father had his first bypass at age 51 and battled heart disease for another 36 years before his death at age 87. His younger brother died a decade ago from heart-related issues.
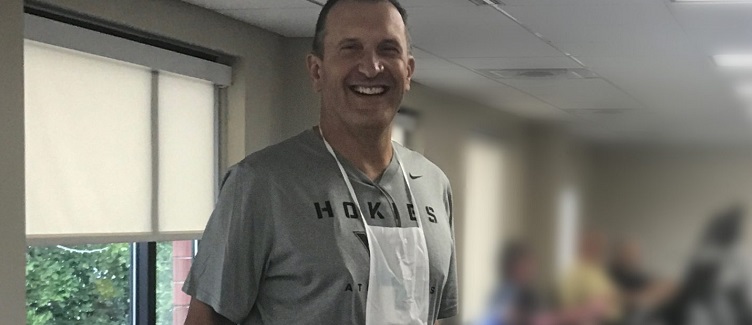
“I thought by working out every day I wouldn’t have the health issues my father and brother faced,” says Bill, 58, the owner of a North Side title insurance company. “I thought I was in pretty good shape.”
The Mars resident swam a mile or more five to six times a week and played racquetball whenever possible. He also golfed during warmer months and played paddle tennis during winter.
Never Miss a Beat!
Stay in the know -- news and updates on UPMC Passavant and its location and services.
Thank you for subscribing!
You can now select the specific newsletters you'd like to receive.
You are already subscribed.
Subscribe to more newsletters in our email preference center.
Sorry, an error occurred. Please try again later.
Get Healthy Tips Sent to Your Phone!
But Bill had just finished his early morning swim last September when he felt a painful pressure in his chest. He took a shower and dressed for a golf outing, but the pain got worse. With the help of a friend, his wife got him into the car and drove straight to UPMC Passavant’s emergency entrance.
Stationed at the metal detector was security guard George Valtchev, who took one look at Bill and instantly recognized his pale, gray face and sweating were signs of a heart attack. When Bill acknowledged he was having chest pains, George quickly alerted the emergency department (ED), put him in a wheelchair, and whisked him inside for immediate care from the cardiac team.
Moments later, an EKG confirmed Bill was having a STEMI — a full-blown heart attack caused by complete blockage of the left anterior descending artery. Often referred to as the “widow maker,” a STEMI is one of the deadliest of heart attacks because the blockage prevents blood from flowing to a large area of the heart. Heart muscle dies if blood flow is not restored quickly.
After stabilizing him in the ED, Bill was moved to UPMC Passavant’s Cardiac Catheterization Lab where interventional cardiologist Bryan Robertson, MD, performed an emergency heart catheterization and stent procedure.
“I thought I might be having a heart attack, but I didn’t think it was massive,” says Bill.
“I’m so grateful for Dr. Robertson — he saved my life. But everyone there at Passavant worked as a team to save me — beginning with George to the folks in ED, to the doctors, and nurses. They were all first class.”
The first person Bill saw after leaving the cath lab was George, who was waiting in the hallway to see him and visited during his hospital stay. The experience created a bond and lasting friendship between them.
Although Bill spent two days in the hospital’s cardiac intensive care unit and another day in the step-down unit, he immediately felt fine after the procedure. “Once the blockage was gone, I felt immediate relief — completely normal,” he says.
Bill also completed six weeks of outpatient rehabilitation at UPMC Passavant-Cranberry. The supervised rehab program, which focused on building cardiovascular endurance and muscular strength while exercising on a treadmill, bike, and other equipment, also helped to encourage him.
“It was reassuring knowing that I was working out safely and my heart was strong enough,” says Bill. “It gave me confidence that I could live my normal life again and resume my routine.”
After his discharge from the hospital, Bill lost 12 pounds just by switching to a heart-healthy diet and eliminating red meat, cheese, peanut butter, and fried foods. He also returned to swimming. He was able to cut his cholesterol medicine in half when his cholesterol levels dropped from 230 to 115.
“I feel great,” says Bill. “My heart attack was a wake-up call. And I’m so grateful to UPMC Passavant for being there for me and giving me this second shot at life.”
Editor's Note: This article was originally published on , and was last reviewed on .
About Heart and Vascular Institute
The UPMC Heart and Vascular Institute has long been a leader in cardiovascular care, with a rich history in clinical research and innovation. As one of the first heart transplant centers in the country and as the developer of one of the first heart-assist devices, UPMC has contributed to advancing the field of cardiovascular medicine. We strive to provide the most advanced, cutting-edge care for our patients, treating both common and complex conditions. We also offer services that seek to improve the health of our communities, including heart screenings, free clinics, and heart health education. Find an expert near you.