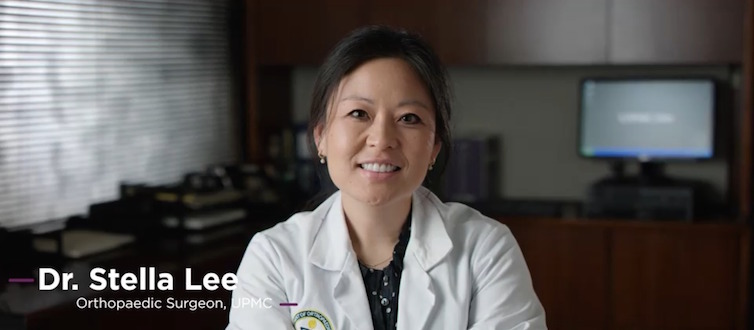
Dr. Stella Lee, an orthopaedic surgeon who specializes in oncology at UPMC Shadyside Hospital and UPMC Hillman Cancer Center discusses a complex surgery used to treat some bone cancer patients as well as collaboration among doctors and the individualized care offered to each patient at UPMC.
Never Miss a Beat!
Subscribe to Our HealthBeat Newsletter!
Thank you for subscribing!
You can now select the specific newsletters you'd like to receive.
You are already subscribed.
Subscribe to more newsletters in our email preference center.
Sorry, an error occurred. Please try again later.
Get Healthy Tips Sent to Your Phone!
Read The Full Podcast Transcript
Tonia Caruso:
Providing specialized orthopaedic care for some of the most complex cases: Welcome to the UPMC HealthBeat Podcast. I’m Tonia Caruso, and joining us right now is Dr. Stella Lee. She is an orthopaedic surgeon who specializes in oncology at UPMC Shadyside and the UPMC Hillman Cancer Center. Dr. Lee, thanks so much for joining us.
Stella Lee:
Thank you for having me. It’s my pleasure to be here.
Tonia Caruso:
So I guess my first question is when it comes to bone cancer, is it always a case of cancer that has spread there from other parts of the body, or can cancer just start independently in the bones?
Stella Lee:
The patients I treat fall into two broad categories: those with metastatic carcinoma or multiple myeloma or lymphoma, which we think of as more of a situation where it metastasized from another location or from a blood primary; and then there’s a second category, broad category, of patients who have bone or soft tissue sarcomas, and those patients have a very, very different type of cancer and require a very specialized surgery, which is where my expertise really comes in, because oftentimes the goal is to try to cure the cancer with a pretty complex surgery.
Tonia Caruso:
And I know you say it’s a complex surgery, but can we give folks an idea of what it entails?
Stella Lee:
Yes. So oftentimes if the tumor started in the bone and there are no other metastatic areas within the body, then we essentially want to cut the entirety of the tumor out, always with a cuff of normal tissue around it to get what we call negative margins. So we don’t want to leave any gross tumor within the patient’s body. And so once the entire segment is removed, oftentimes the next step is to reconstruct the area. So, for example, if I remove the distal half, or the bottom half, of the thigh bone or the femur bone, then I need to put something in there to reconstruct, and oftentimes that requires a very impressive metal prosthesis where the bone used to be.
Tonia Caruso:
Is this something that’s easily detected? What would someone at home, what would they first experience that might lead them, and then lead doctors, to discover that it’s bone cancer?
Stella Lee:
So one would think a mass would be more common, but actually something is bothering the patient — they’re having pain — and oftentimes this may be a night pain and not necessarily related to function. Now, other patients, especially if the tumor gets large enough, they do notice a mass, and then that brings them in. And we subsequently get imaging, as well as a biopsy, to make the diagnosis before proceeding with the necessary treatment.
Tonia Caruso:
Right. And when you do come up with the diagnosis, it’s really a whole team of doctors and medical professionals at the table, and each plan is individualized. Talk a little bit about that and what treatment looks like for a patient.
Stella Lee:
Absolutely. So especially with the diagnosis of sarcoma, you really want to go to a specialized cancer center, and it truly is a multidisciplinary effort. We actually have tumor board once a week, and it’s a multi-service meeting where we all get together and discuss our patients, and this involves the orthopedic oncologists like myself. There are also other cancer surgeon specialists in the room as well. We work very closely with the medical oncologists, and then additionally we have the multidisciplinary care of the pathologists, the radiation oncologists, and also the radiologists who also help us in terms of interpreting the image and long-term follow-up for surveillance to make sure the cancer doesn’t come back or it doesn’t metastasize.
Tonia Caruso:
So, doctor, when cases of COVID-19 first started to emerge in our region, did you change the approach to treatment at all?
Stella Lee:
Fortunately, despite the pandemic, our priority still remained treating our patients with cancer because these are not elective diagnoses or surgeries. And so when a patient had a suspicious mass, we were able to get them into the office to see us right away without delay. The situation in which it impacted our patients a bit was, for example, when a patient has already finished surgery and chemotherapy and/or radiation, and they’re now in what we call the surveillance phase, where we make sure and monitor for any recurrent or metastatic disease. Our health care system in our facility in particular did an excellent job getting telemedicine available to all the providers and most of the patients. We did a transition to trying to use telemedicine, either audio and/or visual, as much as possible. However, we did realize that in certain situations, this is just not feasible and therefore it is important for the patient to actually come back into the office for us to evaluate them in person.
Tonia Caruso:
Why, especially as a physician and a cancer physician, is important to see people in person?
Stella Lee:
There is a lot that cannot be seen virtually. And so especially in the setting of a new diagnosis, it is important for me to actually see the patient, to examine the effect of this new mass or cancer that they might be having, and also for surgical planning. Because for example, if they have a tumor of the leg, it’s important to also examine the lymph nodes and see if there’s anything else that might be worrisome. It’s important to see if there’s any sort of skin discoloration or breakdown because that can affect the surgery. For example, needing additional expertise, such as the plastic surgeon to help us with coverage, or just in terms of the surgery itself, planning so that we anticipate any sort of difficulties that might arise.
Tonia Caruso:
Can you talk about some of the safety precautions in place at the hospital for patients coming in?
Stella Lee:
So at the moment, everybody who comes into the hospital has their temperature taken and are asked just a short series of questions, and then they get a mask. We have started opening up the hospitals a bit more so that now patients can have a visitor while they are admitted. And then especially for surgery, the family member or sometimes members if there’s special permission, can wait in the waiting room together while the surgery is taking place. And that’s definitely a change from even a month ago where we weren’t allowing any visitors into the hospital, which was difficult, understandably, for the patient and families, but it was a necessary precaution to take.
Tonia Caruso:
Would you say that in general the benefits of getting treatment outweigh risks of COVID?
Stella Lee:
In the cancer setting, absolutely.
Tonia Caruso:
And so I know that you deal with specialized cases. Just for anybody who might be watching this that have sort of just general pain, maybe it’s pain in their hip, pain in their knee, when in general would you advise someone that they should see a physician for an evaluation?
Stella Lee:
So one of the most important things to consider is how long has the pain been going on, and is it changing? So oftentimes when we really delve into the details, the patient admits, “Actually, this pain has been going on for years,” and then my next question is, “Well has it changed, and what brought you in?” So if the pain has been consistent for months or years and it is not different, then I think it is safe to wait. However, if it is changing in terms of severity or it’s not responding to treatments that have worked before, like rest, elevation, ice, or anti-inflammatories, then that would be a reason to come in. If there are any other changes, like skin discoloration, if there are any open wounds developing, if there is a limitation in range of motion, those would be reasons to come in.
Tonia Caruso:
And although you’re a surgeon, surgery is not necessary in all cases for all people, correct?
Stella Lee:
Correct.
Tonia Caruso:
No matter what area, what do you finally want to say to patients about getting their health care back on track?
Stella Lee:
We are continually triaging our patients to make sure that the most urgent cases are always seen without delay. Additionally, as we start to open up again, our triage nurses are making an effort to make sure that even the less urgent and perhaps more elective patients do get to see us in a timely fashion. I think the most important thing is to remember that this is an unprecedented time that we’re all going through, and there are going to be measures that remain in place to both protect the patients as well as the hospital staff and the greater community. So I think the most important thing is, yes, please, if you are concerned and have an issue that really should be looked at by a physician or a health care provider, that is absolutely important to do so. However, please also remember that it’s important to continue precautions and work together with us so that we can make sure everyone gets treated adequately and we can deliver the best care possible for our patients.
Tonia Caruso:
Well, Dr. Stella Lee, some great information. Thank you so much for your time today. We certainly do appreciate it.
Stella Lee:
Thank you so much for having me.
Tonia Caruso:
And I’m Tonia Caruso. Thank you for joining us. This is UPMC HealthBeat.
About UPMC Orthopaedic Care
When you are dealing with bone, muscle, or joint pain, it can affect your daily life. UPMC Orthopaedic Care can help. As a national leader in advanced orthopaedic care, we diagnose and treat a full range of musculoskeletal disorders, from the acute and chronic to the common and complex. We provide access to UPMC’s vast network of support services for both surgical and nonsurgical treatments and a full continuum of care. Our multidisciplinary team of experts will work with you to develop the treatment plan that works best for you. Our care team uses the most innovative tools and techniques to provide better outcomes. We also are leaders in research and clinical trials, striving to find better ways to provide our patients care. With locations throughout our communities, you can find a provider near you.