COVID-19, caused by the novel coronavirus SARS-CoV-2, impacts many of the body’s organs. The disease can damage the heart, kidneys, and brain.
The virus can also cause severe lung disease, such as pneumonia, acute respiratory distress syndrome (ARDS), and other conditions. In these cases, the lungs can suffer significant damage such as thickening of lung tissue and scarring.
In rare instances, lung damage from COVID-19 can become irreversible, which may require a single or double lung transplant. This was the case for Dennis Franklin, who received a double lung transplant at the UPMC Lung Transplant Program on Dec. 27, 2021.
For people with severe lung disease, a lung transplant may become their only treatment option. During the procedure, surgeons replace diseased lungs with healthy ones from a deceased organ donor. Doctors may recommend a single or double lung transplant when they can no longer treat lung disease with medications.
Never Miss a Beat!
Subscribe to Our HealthBeat Newsletter!
Thank you for subscribing!
You can now select the specific newsletters you'd like to receive.
You are already subscribed.
Subscribe to more newsletters in our email preference center.
Sorry, an error occurred. Please try again later.
Get Healthy Tips Sent to Your Phone!
Expert Lung Transplant Care
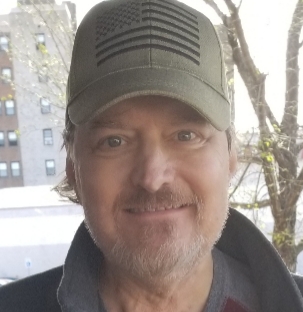 Dennis was on vacation in the summer of 2021 when he came down with COVID-19. His symptoms progressed to the point where he could barely breathe, and one morning, he didn’t wake up.
Dennis was on vacation in the summer of 2021 when he came down with COVID-19. His symptoms progressed to the point where he could barely breathe, and one morning, he didn’t wake up.
The St. Charles, Mo., native was on life support for the remainder of the summer and into fall 2021. His lungs suffered intense damage throughout the process.
As his condition worsened, his doctors knew he needed a lung transplant. Yet Dennis’ condition was complex – not only was he very sick, but not much was known about COVID-19 lung transplants.
“A couple of days after contracting COVID-19, I was diagnosed with lung failure,” Dennis said. “There was a lot of scar tissue on my lungs, and I was very weak.”
A case of his complexity required treatment from leading experts on lung transplant. That’s when he came referred to UPMC.
Who Qualifies for a Lung Transplant
There are more than 2,700 lung transplants performed in the United States every year. Lung transplantation is a lifesaving option for people with:
- Chronic obstructive pulmonary disease (COPD)
- Cystic fibrosis
- Pulmonary fibrosis
- Pulmonary hypertension
The first COVID-19 lung transplant took place in June 2020, and just over two years later, about 10% of lung transplants performed in the U.S. are due to complications from COVID-19.
When COVID-19 causes enough damage that a lung transplant is necessary, it is important to get referred to experienced lung transplant experts as soon as possible. An early referral for lung transplant can allow you to get proper care before your condition worsens.
Dennis transferred to UPMC on Nov. 16, 2021, and came under the care of Pablo Sanchez, MD, surgical director of the UPMC Lung Transplant Program, who would perform his transplant just over a month later.
The Transplant Team and Process
At the UPMC Lung Transplant Program, a team of experts helps candidates like Dennis through every step of their journey. This team includes:
- Lung doctors (pulmonologists) and surgeons
- Psychologists
- Nurses and advanced practice providers (APPs)
- Social workers
If you’re a lung transplant candidate, you’ll first meet with a lung transplant doctor and surgeon to discuss your health and have diagnostic tests like x-rays. They’ll also take blood samples and check your heart and lung function. This evaluation is necessary to determine if it is safe or not to move forward with the transplant.
You’ll need a dedicated caregiver or support person to bring with you to all appointments.
If you get approval for a lung transplant, you’ll be added to the national lung transplant waiting list.
Doctors will discuss your lifestyle and recommend changes while you’re waiting for donor lungs to become available so that your body is in the best health possible before the surgery.
“My care team worked with me every day to get my strength up for the surgery,” Dennis said. “I can’t thank any of them enough.”
The Recovery Process
After his lung transplant, Dennis remained in the hospital under Dr. Sanchez’s care until March 14, 2022. During this time, the team ensured he healed properly from the procedure and started him on physical therapy.
“Things went well after the surgery,” Dennis said. “I could breathe strongly. I only needed oxygen for a few days before I could breathe on my own.”
Immediately after a lung transplant, doctors begin giving recipients immunosuppressant medication so their bodies won’t reject the new lungs.
Dennis’ biggest challenge has been his muscle strength. He’s currently working on pulmonary rehabilitation and physical therapy to build up his stamina after his long hospital stay.
UPMC discharged Dennis in mid-March, and he spent three additional months in Pittsburgh. He attended regular follow-ups with Dr. Sanchez until he was healthy enough to return to his home in St. Charles.
He still occasionally travels to Pittsburgh for follow-ups with the team.
“Dr. Sanchez is just the nicest guy,” Dennis said. “I saw him when I was in Pittsburgh for a bronchoscopy in August (2022). We were both in the cafeteria and I went to go shake his hand — but there was no handshake, there was a hug. There are just not enough words to describe the care I got from him and his team.”
Dennis’ treatment and results are not necessarily representative of similar cases.
About Transplant Services
For more than four decades, UPMC Transplant Services has been a leader in organ transplantation. Our clinicians have performed more than 20,000 organ transplant procedures, making UPMC one of the foremost organ transplant centers in the world. We are home to some of the world’s foremost transplant experts and take on some of the most challenging cases. Through research, we have developed new therapies that provide our patients better outcomes — so organ recipients can enjoy better health with fewer restrictions. Above all, we are committed to providing compassionate, complete care that can change – and save – our patients’ lives. Visit our website to find a provider near you.
