During the first day of school in August 2022, Shawn K., 45, felt a strange sensation along his left side. A behavioral intervention specialist with Sharon City School District, Shawn was meeting with a social skills group to review expectations for the year.
“One minute I was standing up talking to students, and the next minute I felt a numbness radiating down my left arm and hip and into the left side of my neck,” says Shawn. “Then, I felt nauseous.”
Although his symptoms went away quickly, the New Castle, Pa., resident couldn’t shake a lingering uneasiness. At home, he explained to his wife what happened, then called a friend who is a nurse. At her urging, he went to the UPMC Jameson Emergency Department where he was immediately put into stroke protocol.
Never Miss a Beat!
Subscribe to Our HealthBeat Newsletter!
Thank you for subscribing!
You can now select the specific newsletters you'd like to receive.
You are already subscribed.
Subscribe to more newsletters in our email preference center.
Sorry, an error occurred. Please try again later.
Get Healthy Tips Sent to Your Phone!
 Discovering Shawn’s Heart Abnormality
Discovering Shawn’s Heart Abnormality
Shawn’s diagnosis was that he had had a transient ischemic attack (TIA), also known as a “mini-stroke.” TIAs occur when blood flow to the brain suddenly stops for a short time, causing stroke-like symptoms. Unlike a stroke, a TIA does not kill brain cells, which means there is no lasting damage.
After reviewing his symptoms with doctors, Shawn recalled another episode decades earlier. “It happened in my 20s when I was hanging out with friends. I stood up and felt numbness on one side and ringing in my ears,” he says. “It went away quickly, so I didn’t think much about it. But looking back, it was very similar.”
It is uncommon for people under age 55 to experience a stroke, so Shawn’s doctors performed tests to determine the cause. An echocardiogram revealed an abnormality — a hole in his heart known as a patent foramen ovale (PFO).
Advanced Cardiac Treatment
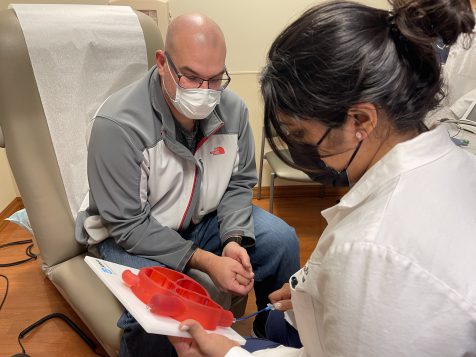
Although Shawn recovered, UPMC recommended surgery to close the hole — a procedure that only a specialist can reform. This then led to his referral to interventional and structural cardiologist Amber Makani, MD, at UPMC Passavant.
According to Dr. Makani, one in four adults has a PFO — a hole between the left and right atria that never closed the way it should after birth. For most people, having one isn’t a problem. But for some, the opening acts as a portal for blood clots to travel from the body through the heart and to the brain, causing a stroke.
“The younger the patient, the more concerned we are that the stroke or TIA was caused by a PFO,” says Dr. Makani. “Shawn already had experienced two TIAs. We wanted to prevent it from happening again.”
Shawn, the father of two young sons, agreed. “It was a no-brainer,” he says. “I have a family. I figured, if I can keep myself healthy and prevent a stroke, then let’s do it.”
Closing the Hole in His Heart
On Nov. 15, Dr. Makani performed the PFO closure during a minimally invasive, catheter-based procedure at UPMC Passavant–McCandless. UPMC cardiologists prefer to use minimally invasive approaches when possible because patients generally have a reduced risk of infection, spend less time in the hospital, and have an overall faster recovery.
After making a small incision in his groin area, Dr. Makani advanced an ultrasound imaging device through a vein up to Shawn’s heart. She then inserted the PFO closure device and guided it up to the heart where it deployed two discs each measuring a little over one inch in diameter straddling each side of the hole. “This stops the abnormal blood flow between the two chambers of the heart,” explains Dr. Makani. “Once the catheter is removed, the procedure is complete.”
Shawn’s surgery was complete in less than an hour. After two hours in recovery for observation and an echocardiogram that confirmed the device was still positioned properly, Shawn returned home.
“The whole experience was great. Dr. Makani and her team explained everything and answered all my questions. It really put me at ease,” says Shawn.
This treatment is one of the latest examples of the expanded heart and vascular care and innovative technology now available at UPMC Passavant — making it convenient for patients living in Pittsburgh’s northern suburbs and beyond who don’t need to travel into the city for advanced care.
Find a heart and vascular provider.
About Heart and Vascular Institute
The UPMC Heart and Vascular Institute has long been a leader in cardiovascular care, with a rich history in clinical research and innovation. As one of the first heart transplant centers in the country and as the developer of one of the first heart-assist devices, UPMC has contributed to advancing the field of cardiovascular medicine. We strive to provide the most advanced, cutting-edge care for our patients, treating both common and complex conditions. We also offer services that seek to improve the health of our communities, including heart screenings, free clinics, and heart health education. Find an expert near you.

 Discovering Shawn’s Heart Abnormality
Discovering Shawn’s Heart Abnormality