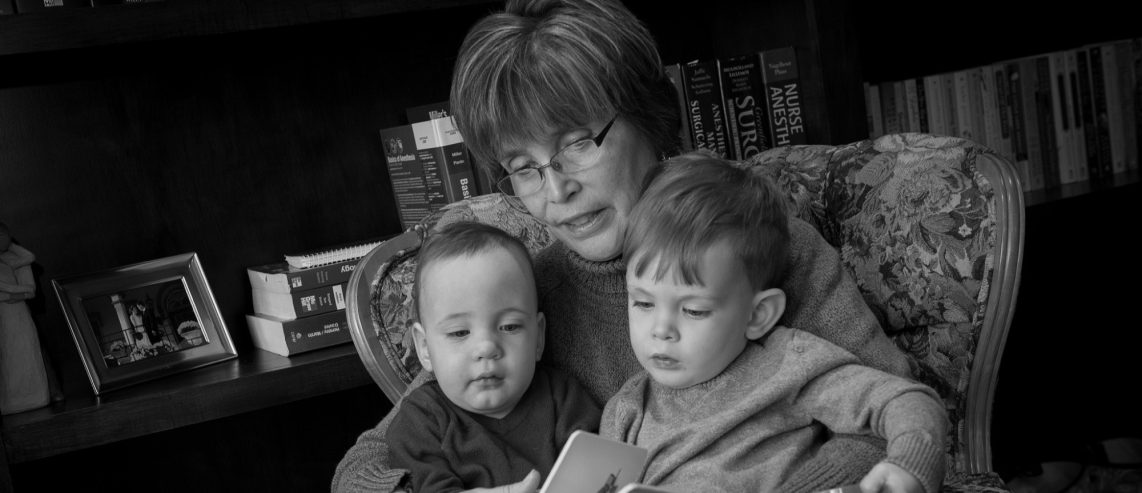
Kay, a 70-year-old mother of three and grandmother of five from north central Pennsylvania, led a busy lifestyle.
But the worsening effects of urinary incontinence began to ruin her ability to do her job, her capacity to play with her grandsons, and, eventually, her desire to even leave her house.
For older adult women with active lifestyles, few things are more disheartening than urinary incontinence. But there are options for treating this condition.
In Kay’s case, Botox® injections helped her overcome her problems.
Never Miss a Beat!
Subscribe to Our HealthBeat Newsletter!
Thank you for subscribing!
You can now select the specific newsletters you'd like to receive.
You are already subscribed.
Subscribe to more newsletters in our email preference center.
Sorry, an error occurred. Please try again later.
Get Healthy Tips Sent to Your Phone!
Cramping Your Lifestyle
Over several years in her early and mid-60s, Kay’s urinary urgency incontinence progressed rapidly. It got to the point where she was frequenting the bathroom a few times per hour and was using four incontinence pads per day.
Soon, even a pad alone wasn’t enough for her to be confident. She’d wear an adult diaper with the pad for extra protection.
“I don’t think I can explain what it’s like to be standing there talking to people at work trying to pay attention, and all you can think about is that you don’t want to have an embarrassing leak situation,” Kay remembers.
“Talk about cramping your lifestyle.”
Kay, who had worked for more than 30 years as a surgical technician, sought help initially with her primary care provider. She was referred to Dr. Glenn Bloiso, MD, a urologist at UPMC Williamsport.
“I knew who Dr. Bloiso was from working in the operating room and really liked him,” Kay says. “Interestingly, as he was taking my medical history, he asked me if I had Parkinson’s — because incontinence can be a symptom of Parkinson’s — and I said, ‘No.’ But a little more than a year later, I was diagnosed with Parkinson’s.”
Intense Urgency
At that visit, Dr. Bloiso diagnosed detrusor muscle instability — spasm of the detrusor muscle of the bladder — as the cause of Kay’s incontinence. This condition is often known as overactive bladder (OAB) syndrome.
Up to 40% of American women live with varying degrees of OAB symptoms. Kay describes her feeling as an intense urgency to go right away, even if she just went less than an hour ago. These sensations went on all day.
The detrusor is the muscle that wraps around the outside of the bladder. It contracts during urination to push the urine out of the bladder and into the urethra, the tube that allows urine to leave the body. It then relaxes to allow the storage of urine in the urinary bladder until it is time to void again.
The cause of detrusor muscle spasms is found in only about 10% of patients; in 90%, the cause is idiopathic or unknown.
As the first course of treatment, Dr. Bloiso recommended a noninvasive approach using a topical anticholinergic medication applied as a gel to the skin.
“The gel seemed to help at first, but after a year, my situation actually got worse,” Kay says. “So Dr. Bloiso recommended the Botox treatment.”
Botox for the Bladder
If Botox for the bladder sounds odd, consider the principle.
Botox has been used for decades to relax the muscles of the face that produce facial wrinkles. The Food and Drug Administration (FDA) approved using Botox injections into the detrusor muscle to relax overactive bladder symptoms in 2011.
Dr. Bloiso performed Kay’s first Botox procedure in 2018. The procedure uses a cystoscope, a thin tube with a camera that is advanced into the bladder through the urethra, the opening in the body where urine is released. Although some numbing agents are used during the procedure, the patient is awake the whole time.
A few days before the procedure, Kay underwent a sterile catheterization to ensure there was no infection. She took a preventive dose of oral antibiotics the day before the treatment.
On the day of the procedure, Kay described the nurses as “wonderful.” They walked her through the whole process and helped her to relax.
During the cystoscopy procedure, Dr. Bloiso first administered a numbing agent. Then he made a series of injections with 100 units of Botox into the detrusor muscle.
Best Gift Ever
Dr. Bloiso cautioned her that the Botox could take up to a week or more to show any signs of improvement. But Kay’s improvement was immediate.
“It was near the holidays when I first had it done because all I can remember was telling Dr. Bloiso that this was the best Christmas gift I ever received!” Kay recalls.
Each of the Botox procedures lasts about five to six months and must be repeated to maintain the effects.
Since her initial Botox treatment in 2018, Kay has retired from her job. But she is enjoying her retirement and her ability to spend time with her grandsons.
Her Parkinson’s diagnosis has caused her to slow down a bit, she says.
But since the urge to go is gone, she’s been able to go line dancing and return to other activities she once enjoyed. She can play with her grandkids and exercise with a friend who is a personal trainer.
Kay is thankful that the Botox procedures have improved her quality of life, which has helped her keep her Parkinson’s in check.
“They’re life changing,” she says.
For more information about treatments of overactive bladder, visit UPMC’s website.
About Urology
The UPMC Department of Urology offers a wide variety of specialized care for diseases of the male and female urinary tract and the male reproductive organs, including erectile dysfunction, kidney stones, urinary incontinence, prostate cancer, and more. We have a multifaceted team of physicians and researchers working together to provide the best care to both children and adults. Our team is nationally renowned for expertise in highly specialized technologies and minimally invasive surgical techniques. To find a provider near you, visit our website.