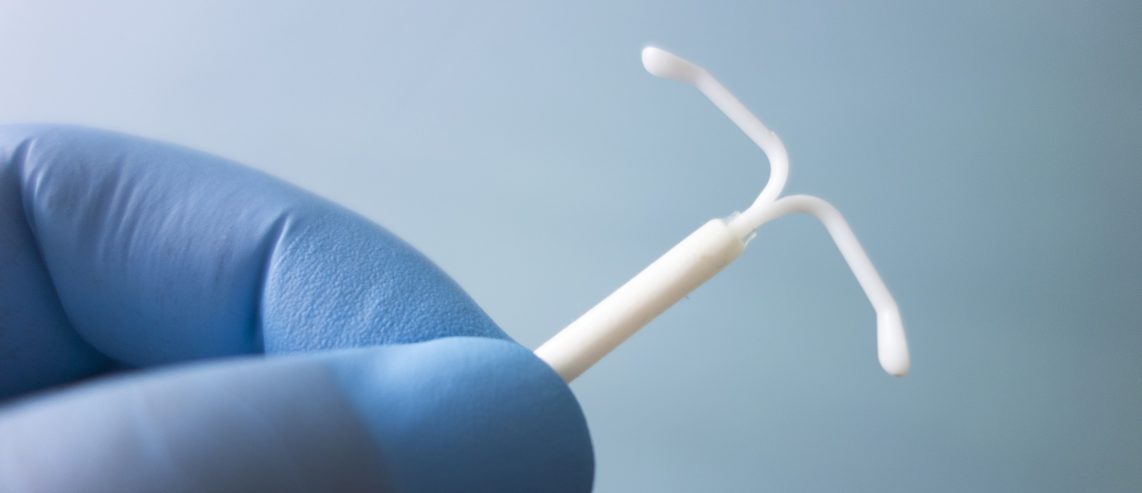
For people with female reproductive systems, one of the most effective types of birth control is an intrauterine device (IUD). Here’s what you should know about the different types of IUDs.
What’s an IUD?
IUD stands for intrauterine device. It’s a small piece of plastic or some with small copper wires used to prevent pregnancy. A doctor or nurse inserts the device into your uterus through your cervix.
Depending on the IUD, they last from 3 to 10 years. After this time, you need to have them removed. You can go off birth control if you’re looking to get pregnant, use another birth control method, or have another IUD inserted.
You can have the IUD taken out earlier if you want. But only a doctor or other trained health care worker should remove your IUD.
IUDs are one of two types of long-acting reversible contraceptives (LARC). The other LARC method is hormonal implants.
LARCs are the second most effective type of birth control after sterilization surgery. That’s according to the U.S. Department of Health and Human Service’s Office on Women’s Health.
Never Miss a Beat!
Subscribe to Our HealthBeat Newsletter!
Thank you for subscribing!
You can now select the specific newsletters you'd like to receive.
You are already subscribed.
Subscribe to more newsletters in our email preference center.
Sorry, an error occurred. Please try again later.
Get Healthy Tips Sent to Your Phone!
How IUDs Work
IUDs are more than 99% effective at preventing pregnancy, according to Planned Parenthood. IUDs work by:
- Preventing your ovaries from releasing eggs.
- Preventing sperm from getting to the eggs.
- Making implantation of the egg in the uterus unlikely.
With an IUD, you don’t need to remember to take a pill every day. Once the IUD is in your uterus, there is nothing else you need to do to prevent pregnancy.
You need a prescription from your doctor or gynecologist to get an IUD. They will place the IUD during an appointment in their office or clinic.
After insertion, you may need a follow-up visit to check the IUD placement. In rare cases, IUDs can move and puncture your uterus.
Different Types of IUDs
When it comes to IUDs, you have two types to choose from:
- Copper IUDs
- Hormonal IUDs
Both types of IUDs work equally well at preventing pregnancy. In any given year, less than 1 in 100 people with an IUD have an unplanned pregnancy. That’s according to the Office on Women’s Health.
Neither type of IUD protects against sexually transmitted diseases (STIs) like HIV. To protect against STIs, use a condom.
Below are the key differences between copper and hormonal IUDs.
Key facts about copper IUDs
Of the two types of IUDs, copper IUDs last the longest. They can last up to 12 years before your doctor needs to remove or replace the device. Paragard is the brand name for the copper IUD currently on the market in the U.S.
Copper IUDs do not contain hormones. They are T-shaped devices wrapped in copper wire.
Side effects of copper IUDs
Copper IUDs can cause some side effects. Common side effects of a copper IUD include:
- Cramping for a few days after insertion.
- Bleeding between periods.
- Having heavier periods.
- Missing periods.
- More often or more intense menstrual cramps.
Benefits of copper IUDs
Copper IUDs work right after insertion. Because of this, they can also work as emergency contraception if inserted within five days of having unprotected sexual intercourse. Copper IUDs are more effective at preventing pregnancy than emergency contraceptive pills, according to KFF.
Key facts about hormonal IUDs
Hormonal IUDS are also called LNG-IUDs. They release small amounts of the progestin hormone levonorgestrel each day. Hormonal IUDs are the most commonly used IUD.
Depending on the brand, these hormonal IUDs can last 3 to 8 years before your doctor needs to remove or replace them. There are four brands of hormonal IUDs available.
- Mirena is effective for up to 8 years.
- Skyla is effective for up to 3 years.
- Lilleta is effective for up to 8 years.
- Kyleena is effective for up to 5 years.
Unlike copper IUDs, hormonal IUDs take time to start working after insertion, so they do not work as emergency contraception. Doctors often recommend using a condom as a backup method of birth control during the first month of having one.
Side effects of hormonal IUDs
Common side effects of hormonal IUDs include:
- Breast tenderness.
- Depression.
- Headaches.
- Irregular periods during the first few months.
- Lighter periods.
- Missed periods.
- Nausea.
- Ovarian cysts.
Benefits of hormonal IUDs
Like all hormonal birth control methods, hormonal IUDs may help if you struggle with heavy, painful, or long-term bleeding. Doctors may also prescribe hormonal IUDS for heavy menstrual periods. When using a hormonal IUD for heavy bleeding, doctors will remove it sooner, often after 5 years.
Other benefits of hormonal birth control, including hormonal IUDs, may include:
- Fewer menstrual cramps.
- Less acne.
- More regular periods.
- Lighter periods.
In general, oral hormonal birth control can also lower your risk of:
- Colon cancer.
- Endometrial cancer
- Iron-deficiency anemia.
- Ovarian cancer.
Is Copper IUD or Hormonal IUD Better?
Neither the copper IUD nor the hormonal IUD is always better. Both have pros and cons depending on the person looking to prevent pregnancy.
Which is better is a personal question that depends on your desires, goals, and medical history.
How To Tell Which IUD Is Right For You?
Your doctor or gynecologist can help you choose an IUD. They will go over your complete medical history to figure out which is right for you.
Health Problems Related to IUDs
Both types of IUDs can also cause some serious health risks. These include:
Ectopic pregnancy
Both copper and hormonal IUDs can slightly increase your risk of an ectopic pregnancy, a serious health issue that requires immediate treatment. Ectopic pregnancies are when a fertilized egg implants somewhere outside of the uterus. Most ectopic pregnancies implant in one of the fallopian tubes.
Pelvic inflammatory disease
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs caused by an STI. In very rare cases, IUD insertion in women with an asymptomatic STI can trigger PID.
Testing and prompt treatment for the STI can reduce the risk of developing PID during an IUD insertion, research in the journal Obstetrics & Gynecology shows.
Left untreated, PID can cause long-term pelvic pain and problems getting pregnant and during pregnancy. The most common symptom of PID is pain in the lower abdomen or belly. Other signs and symptoms include:
- Fever of 100.4° F or higher.
- Irregular periods.
- Painful sex.
- Pain when urinating.
- Upper right abdomen pain, though this is rare.
- Vaginal discharge that may smell foul.
Punctured uterus
In rare cases, the IUD can move from where it’s inserted and puncture the uterine wall.
When to call your doctor?
Call your doctor right away if you:
- You have severe pain or fever after getting an IUD.
- You miss a period or get a positive pregnancy test.
- You have abdominal pain.
- Your IUD comes out.
Sources
Birth Control Methods. U.S. Department of Health and Human Services. Office on Women's Health. Link.
Pelvic Inflammatory Disease. Office on Women's Health. Link.
KFF. Women's Health Policy. Intrauterine Devices (IUDs): Access for Women in the U.S. Link. Sept. 2020. Link.
How Effective Are IUDs. Planned Parenthood. Link.
Liletta. Link.
Mirena. Link.
Skyla. Link.
Kyleena. Link.
Paragard. Link.
Sufrin CB, Postlethwaite D, Armstrong MA, Merchant M, Wendt JM, Steinauer JE. Neisseria gonorrhea and Chlamydia trachomatis screening at intrauterine device insertion and pelvic inflammatory disease. Obstet Gynecol. 2012;120(6):1314-1321. doi:10.1097/aog.0b013e318273364c
About UPMC Magee-Womens
Built upon our flagship, UPMC Magee-Womens Hospital in Pittsburgh, and its century-plus history of providing high-quality medical care for people at all stages of life, UPMC Magee-Womens is nationally renowned for its outstanding care for women and their families.
Our Magee-Womens network – from women’s imaging centers and specialty care to outpatient and hospital-based services – provides care throughout Pennsylvania, so the help you need is always close to home. More than 25,000 babies are born at our network hospitals each year, with 10,000 of those babies born at UPMC Magee in Pittsburgh, home to one of the largest NICUs in the country. The Department of Health and Human Services recognizes Magee in Pittsburgh as a National Center of Excellence in Women’s Health; U.S. News & World Report ranks Magee nationally in gynecology. The Magee-Womens Research Institute was the first and is the largest research institute in the U.S. devoted exclusively to women’s health and reproductive biology, with locations in Pittsburgh and Erie.